ABSTRACT
While an underweight prevalence was once more than double that of obesity, now more people are obese than underweight. Obesity is one of the leading causes of preventable death in the world. There are an estimated 2,100,000,000 obese people worldwide and that number is forecast to grow to 51% of the world’s population by 2030. Escalating obesity-related disease costs threaten to bankrupt the world’s healthcare systems.
The author reviews some of the causes for the increasing prevalence of this disease, identifies opportunities to intervene to prevent its progression, and discusses possible methods that may avert further increase in the overall prevalence of obesity in the general population.
VIEWPOINT
2,100,000,000 people or nearly 30% of all people about the globe are obese with the U.S. population being the most obese. Not one country has achieved success in reducing obesity rates.1 Although some models suggest leveling off may limit the prevalence to a more modest 42%, linear trends forecast 51% of the world’s population is forecast to be obese by 20302. Obesity related diseases include gastric reflux, sleep apnea, hypertension, hyperlipidemia, autoimmune diseases and cancer, heart disease, strokes, and most significantly type 2 diabetes mellitus. In a report published November 20, 2014, McKinsey Global Institute estimated worldwide annual Obesity related disease costs reached $2,000,000,000 and are forecast to grow by 9.6% annually to $17,000,000,000 in 2030, threatening to bankrupt national healthcare systems.
In the vast majority of circumstances, diet and counseling are less successful than weight loss surgery as long-term solutions3,4 and successful treatment requires a multidisciplinary approach.5 However, in spite of the increasing obesity problem, the number of bariatric surgeries performed annually remains limited to a very small portion of the afflicted population.
Established surgical options are either restrictive or bypass in nature. These surgeries involve cutting into the bowel, rearranging the body’s alimentary plumbing or leaving behind a foreign body to force the patient to eat less or make food wind up in the toilet incompletely digested, with potential of creating nutritional cripples. The number of bariatric surgeries has plateaued with annual costs exceeding $1,500,000,0006 and was estimated at approximately 196,000 by the American Society for Metabolic and Bariatric Surgery for 2015 with Roux-en-Y and gastric banding losing popularity in favor of gastric sleeves. They reported revisions have more than doubled between 2011 and 2015 and comprise almost 14% of all such surgeries. The low plateau evidences patient and physician dissatisfaction with the costs, risks and long-term sequelae of current surgical options.
Following funding infusions for product development to meet the growing unmet need, multiple technologies have recently attained U.S. FDA. Premarket Approval or are on the cusp to do so, positioning the markets for significant growth.7,8 .These devices and procedures provide lower cost, less invasive solutions and involve different mechanisms of action. They may be grouped into those which will be introduced as temporary diet training aides, and those with potential of being a more permanent solution. Most physicians are inclined to prefer a safer, permanent solution to temporary ones that may potentially increase rather than decrease obesity costs.
LAP-BAND® (Apollo Endosurgery) is legacy adjustable gastric band which is a minimally invasive laparoscopic weight loss device with both FDA approval and broad-based insurance coverage. However LAP-BAND®, which is approved for long-term use, has a declining market share due to patients not losing weight, regaining weight lost, significant revisions or complications9, or patients not liking draconian portion limits.
The FDA has approved the Orbera Intragastric Balloon System (Apollo Endosurgery) and ReShape Integrated Dual Balloon System (ReShape Medical) for up to 6 months of use in adults with a BMI of 30-40 who have not been able to maintain weight loss with a weight loss program and, for ReShape, who have at least one obesity-related comorbidity.10,11 Similar products such as Satisphere™ (Endosphere) are in the pipeline and proceeding with safety studies. Nausea and vomiting experienced by some patients and the slim possibility of the 35% fatal Boerhaave’s syndrome may hinder acceptance12,13. Furthermore, the stomach is likely to dilate around the device countering its volume filling effect and leading patients to eat more to be satiated after removal, regain any lost weight, and possibly be worse off than before the procedure.
Temporary malabsorptive alternatives which may remain in place no more than 12 months include intraluminal shunts such as Endobarrier™ (GI Dynamics) and TIPS™ (BAROnova)14. Safety studies of the former for its PMA have been completed and safety studies for the latter are in process. Since any internal shunt to cause food to bypass digestive enzymes will not peristalse like bowel, it will eventually occlude and need to be replaced or removed.15 Furthermore, intestinal villi may hypertrophy to compensate and become more absorptive distal to those bypassed, not only leading to eventual weight regain but leaving the patient worse off than before the procedure.
Other novel approaches approved for long term use include attempts to stimulate CN X to induce satiety or emptying. These include Abiliti™ (IntraPace) and VBLOC™ (EnteroMedics). The Maestro rechargeable system for VBLOCK just received approval16. The These electro-stimulation devices suffer not only from their high costs (approximately $20,000 USD) and the necessity of nightly re-charging, but from the fact that they pose foreign body risks. The brain’s neuroplasticity also makes it not likely that it will habituate to the neural stimulation over time.
In the past decade, we have learned that it is the visceral fat within the abdomen that is responsible for all the morbidity associated with obesity – sleep apnea and gastric reflux simply by bulk, and type 2 diabetes and hypertension, autoimmune diseases, and cancers by virtue of the cytokines or cellular hormones it secretes.17,18 Omental fat is one location for this fat. Removing it in conjunction with a LAP-BAND® procedure has produced an additive beneficial effect.19,120 Omentectomy has been shown to have an added a beneficial effect when carried out in conjunction with roux-en-Y bypass procedures but only if they were less aggressive and omentectomy was performed more completely.21 Even if performed laparoscopically, omentectomy literally requires cutting it out and is not a totally benign procedure.
Up until now it was not safe or efficient to remove the visceral fat in the mesentery of the small bowel that endocrinologists and gastroenterologists believe to be may be more metabolically active.22 The thickness of this mesentery has been shown to be directly correlated not just to the severity of metabolic disease23 but to the intimal thickening of patient’s carotid arteries, providing a clear-cut indicator of the likelihood of vascular disease and stroke.24 Removal of that mesenteric fat safely and efficiently may now be possible, providing a safer and more permanent minimally invasive solution rather than just a temporary one and one without undesirable permanent sequelae such as draconian portion limits, diarrhea, the need for frequent lab tests, or nutritional impairment.
Using an endoscopic generation of a technology originally developed to facilitate safer and less onerous liposuction, (Twin Cannula Assisted Liposuction or “TCAL”), a tube-within-a-tube technology that does not require the surgeon to actively stroke or reciprocate an aspirating cannula24, the EVL® device under development (BioSculpture Technology, Inc.) will permit laparoscopic assessment of which of intraabdominal fat is the most noxious and safely and efficiently remove it. Unlike all other new less invasive bariatric interventional alternatives, the results of EVL are expected to be permanent. EVL will not require cutting into the bowel or stomach, rearranging the body’s alimentary plumbing, leaving behind a foreign body, or have any danger of creating malabsorption syndromes and nutritional cripples. Clinical testing and regulatory approvals are yet to be obtained and the procedure is not yet available, but if visceral lipectomy in humans attains postsurgical weight loss and metabolic improvement similar to that observed in animals22, it holds potential of not just becoming a first line procedure in the treatment of established metabolic syndrome and type 2 diabetes, but of widening patient selection to affect the course of the disease.
The world health organization recognized obesity as a disease in 1997. Obesity was officially classified as a disease by the Centers for Medicare and Medicaid Services (CMS) in 2004 and the AMA in 2013, thus removing a major barrier to access to medical treatment for obese patients in the U.S.. In 2006, and again in 2012, CMS expanded coverage to include more types of devices and procedures, further improving patient access to care. While CMS pays for only 20% of bariatric procedures for obesity, it sets the bar for U.S. insurers to follow.
Clinical data about obesity related co-morbidities heightens governmental interest in obesity. The U.S. regulatory environment for obesity companies is favorable with access to the Expedited Access Pathway. The FDA enacted a benefit-risk paradigm for clinical trial design of obesity devices and is supportive of advancing new technologies to the commercial markets for obesity-related devices and procedures. U.S. President-elect Donald Trump has expressed a willingness to further loosen of F.D.A policy that may further speed approvals.
An obese mother is five times more likely to have an obese child.25 As visceral adiposity starts in utero, this child will be born with a greater proportion of visceral fat.26 25% of children in the U.S. are already obese. It’s not only well established that visceral fat has been shown to be a risk factor for metabolic syndrome but that mesenteric thickening with visceral fat is directly correlated to carotid intimal thickening. Visceral fat causes sleep apnea and gastric reflux simply because of bulk and secretes noxious cytokines that are responsible for all of the morbidities of obesity – resistin for type 2 diabetes, angiotensin for hypertension, tumor necrosis factor and interleukins for inflammatory vascular disease, and neuropeptide-Y for insatiable hunger. It is a noxious cytokine factory.
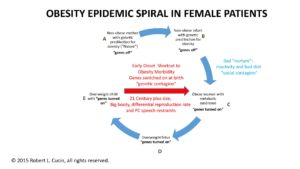
Opportunities for intervention and a treatment algorithm may be developed pursuant to the model for the tightening spiral of obesity prevalence depicted in Figure 1. A non-obese mother with or without a genetic predilection for obesity (“nature”) can enter the cycle and give birth to a non-obese infant. Obesity is more prevalent (43%) in certain ethnicities such as Blacks and Hispanics. The mother cannot control her genetic predisposition, but she can control the state of the epigenetic switches at the time of conception27. She can also control whether she chooses to increase on the hard-coded genetic propensities towards obesity in her choice of a mate if she receives preconception counseling. A sedentary life style and bad diet (“nurture”), and any inherited genetic predilection can convert this child into an obese adolescent with an excess of visceral fat and epigenetic metabolic switches for the noxious visceral fat cytokine factory switched on. Counseling to change dietary and life style as well as any pharmacologic or genetic therapies that may be developed may prevent the child from becoming an adult obese adult pregnant mother likely to have an obese child. If the obese adolescent becomes an obese pregnant mother, the obesity spiral will tighten until the McKinsey’s Global Institute’s projection of 50% of the world’s population becoming obese by 2030 is realized. If we can prevent that mother from being obese, we can uncoil the tightening spiral and reverse this trend.
If EVL proves safe and effective, it may provide a means of preventing that child from becoming an obese mother when counseling is ineffective. From studying the mesenteric fat removed, EVL can allow us to learn whether these patients genetically prone to obesity have numerically more adipocytes present or just adipocytes more full with fat that are actively secreting the adipocytokines that cause metabolic syndrome. It will also allow us to identify the precise location of the most metabolically active cytokine factories. The ileal mesentery is a highly suspect offender given its involvement (“creeping fat”) with such autoimmune diseases as Crohn’s disease.28
An area for future study is whether a father with a family history of obesity will have an increased likelihood of an infant be obese if he himself is obese at the time of conception, presumably with his epigenetic obesity switches turned on. If so, this would present an opportunity on the male side as well to interrupt the spiral with counseling or EVL.
There general denial by one-third of the general population that obesity is a disease which shortens lives and reduces their quality. There is still the associated stigma at least in some people’s minds that obesity is because of weak will power or gluttony. There is not general knowledge on the public of genetic propensities and that after establishment obesity is homeostatically maintained by powerful cytokines such as ghrelin, neuropeptide-Y, and resistin causing hunger and preventing insulin from allowing sugar to enter cells to satisfy their metabolic needs. Those homeostatic mechanisms are responsible for the frequent failure of diet and counseling. New medical devices under development may permit new less invasive and safer approaches to the obesity problem such as EVL that may allow us to reduce the reverse the trend towards an increasing prevalence of obesity in each subsequent generation, but success will also depend upon changes in our lifestyles and diets. More importantly it will require broad and early public education and counseling with emphasis that obesity is a treatable, inheritable disease which shortens and reduces the quality of the lives of those afflicted.
REFERENCES
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet August 2014; 384(9945):766-781. doi: 10.1016/S0140-6736(14)60460-8.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012 Jun;42(6):563-70. doi: 10.1016/j.amepre.2011.10.026.
- Panosian J, Ding SA, Wewalka M, Simonson DC, Goebel-Fabbri A, Foster K, Halperin F4, Vernon A, Goldfine AB. Physical Activity in Obese Type 2 Diabetes After Gastric Bypass or Medical Management. .Am J Med. 2016 Aug 20. pii: S0002-9343(16)30796-3. doi: 10.1016/j.amjmed.2016.07.019.
- Weiner, R. A., et al. (2010). Indications and principles of metabolic surgery. U.S. National Library of Medicine. 81(4) pp.379-394.
- Montesi L, Ghoch ME, Brodosi L, Calugi S,Marchesini G, Grave RD. Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes. 2016; 9: 37–46.. doi: 10.2147/DMSO.S89836.
- Livingston EH. The incidence of bariatric surgery has plateaued in the U.S. .Am J Surg. 2010 Sep;200(3):378-85. doi: 10.1016/j.amjsurg.2009.11.007. PMCID: PMC2923252
- Zhu C, Pryor AD. Innovations in Bariatric Surgery. Surg Technol Int. 2015 Nov;27:129-35.
- Stacy A. Brethauer SA, Chang, J, Neto MG, Greve JW, M.D. Gastrointestinal devices for the treatment of type 2 diabetes. Surg Obesity Rel Dis 2016 12(6): 1256–1261. doi: /10.1016/j.soard.2016.02.031
- Altieri MS, Yang J, Telem DA et al. Lap band outcomes from 19,221 patients across centers and over a decade within the state of New York. Surg Endosc. 2016 May;30(5):1725-32. doi: 10.1007/s00464-015-4402-8.
- Kumar N. Weight loss endoscopy: Development, applications, and current status. World J Gastroenterol. 2016 Aug 21;22(31):7069-79. doi: 10.3748/wjg.v22.i31.7069.
- ReShape and Orbera–two gastric balloon devices for weight loss. Med Lett Drugs Ther. 2015 Aug 31;57(1476):122-3. PMID: 26305524 [No authors listed]
- Ponce J, Woodman G, Swain J, et al. The REDUCE pivotal trial: a prospective, randomized controlled pivotal trial of a dual intragastric balloon for the treatment of obesity. Surg Obes Relat Dis. 2015 Jul-Aug;11(4):874-81. doi: 10.1016/j.soard.2014.12.006. Epub 2014 Dec 16.
- Yorke E, Switzer NJ, Reso A, Shi X, de Gara C, Birch D, Gill R, Karmali S. intragastric Balloon for Management of Severe Obesity: a Systematic Review. Obes Surg. 2016 Sep;26(9):2248-54. doi: 10.1007/s11695-016-2307-9.
- Kumar N Endoscopic therapy for weight loss: Gastroplasty, duodenal sleeves, intragastric balloons, and aspiration. World J Gastrointest Endosc. 2015 Jul 25;7(9):847-59. doi: 10.4253/wjge.v7.i9.847.
- Rohde U EndoBarrier gastrointestinal liner. Delineation of underlying mechanisms and clinical effects. .Dan Med J. 2016 Nov;63(11). pii: B5309.
- Hwang SS, Takata MC, Fujioka K, Fuller W. Update on bariatric surgical procedures and an introduction to the implantable weight loss device: the Maestro Rechargeable System.Med Devices (Auckl). 2016 Aug 17;9:291-9. doi: 10.2147/MDER.S106223. eCollection 2016.
- Auzumdar R1, Allison DB, Huffman DM, Ma X, et al.. Visceral adipose tissue modulates mammalian longevity. Aging Cell. 2008 Jun;7(3):438-40. doi: 10.1111/j.1474-9726.2008.00391.x.
- Huffman DM1, Barzilai N. Role of visceral adipose tissue in aging. Biochim Biophys Acta. 2009 Oct;1790(10):1117-23. doi: 10.1016/j.bbagen.2009.01.008.
- Thörne A, Lönnqvist F, Apelman J, Hellers G, Arner P. A pilot study of long-term effects of a novel obesity treatment: omentectomy in connection with adjustable gastric banding Int. Int J Obes Relat Metab Disord. 2002 Feb;26(2): 193-199.
- Andersson DP, Thorell A, Löfgren P, et al. Omentectomy in addition to gastric bypass surgery and influence on insulin sensitivity: a randomized double blind controlled trial. Clin Nutr. 2014 Dec;33(6):991-6. doi: 10.1016/j.clnu.2014.01.004.
- Herrera MF, Pantoja JP, Velázquez-Fernández D et al. D Potential additional effect of omentectomy on metabolic syndrome, acute‐phase reactants, and inflammatory mediators in grade III obese patients undergoing laparoscopic Roux‐en‐Y gastric bypass: a randomized trial. Diabetes Care. 2010 Jul;33(7):1413-8.
- Catalano KJ1, Stefanovski D, Bergman RN. Critical role of the mesenteric depot versus other intra-abdominal adipose depots in the development of insulin resistance in young rats. Diabetes. 2010 Jun;59(6):1416-23. doi: 10.2337/db08-0675. Epub 2010 Mar 18.
- Andrade LJ, Melo PR, Paraná R, Daltro C. Grading scale of visceral adipose tissue thickness and their relation to the nonalcoholic fatty liver disease. Arq Gastroenterol. 2014 Apr-Jun;51(2):118-22.
- Liu KH, Chan YL, Chan WB, Chan JC, Chu CW. Mesenteric fat thickness is an independent determinant of metabolic syndrome and identifies subjects with increased carotid intima-media thickness. Diabetes Care. 2006 Feb;29(2):379-84. PMID: 16443891
- Becker DG, Cucin RL Chapter: Powered Liposuction. Powered Instrumentation in Surgery, Singular Publishing Group, San Diego, California, 2000.
- Godfrey KM, Reynolds RM, Prescott SL, et al. Influence of maternal obesity on the long-term health of offspring.Lancet Diabetes Endocrinol. 2016 Oct 10. pii: S2213-8587(16)30107-3. doi: 10.1016/S2213-8587(16)30107-3.
- Jovanovic-Peterson L, Crues J, Durak E, et al. Magnetic resonance imaging in pregnancies complicated by gestational diabetes predicts infant birthweight ratio and neonatal morbidity. Am J Perinatol. 1993;10(6):432-437.
- Adamo KB, Zachary M. Ferraro ZM, Brett KE. Can We Modify the Intrauterine Environment to Halt the Intergenerational Cycle of Obesity? Int J Environ Res Public Health. 2012 Apr; 9(4): 1263–1307. doi: 10.3390/ijerph9041263
- Kredel LI, Siegmund B. Adipose-tissue and intestinal inflammation – visceral obesity and creeping fat. Front Immunol. 2014 Sep 24;5:462. doi: 10.3389/fimmu.2014.00462. eCollection 2014.24.

Patients tend to take remarks concerning their weight really insidiously instead of seeing it as the health danger that it is. Numerous doctors don’t desire to insult their patients and/or make them feel negative about themselves at all. Some physicians believe that food choice and fat burning counseling is not within the extent of their practice. Typically, diet and weight-loss strategies are topics more completely studied in the area of dietetics or nourishment; additionally, an individual’s insurance coverage might not pay for excessive weight screening, or weight management programs, and a person may not want to pay the co-pay costs. – http://www.gastricbypassalternatives.com
“Political” correctness about the topic of Obesity kills. Insurance does cover effective bariatric surgical solutions, but pre-approval may be necessary and currently such operations are generally reserved for the morbidly obese and brittle diabetics in many cases. Given the drain on healthcare systems, and insurance companies from Obesity-related diseases, of which the most significant is Type 2 Diabetes with its amputations, renal failure requiring dialysis and retinopathy blindness, that will change! Kudos for anything you can do to help, but diet and exercise by itself is successful over the long term for very few patients. This is because those signet-shaped fat-cells may be squashed, but they are waiting for that ingested dose of sugar and salt to swell into secretory mode putting out resistin that neutralizes insulin and neuropeptide-Y that acts right on the hunger center in the brain! Removing those visceral fat cells is the only permanent solution once the body has attained homeostasis to the presence of belly fat!
Excellent site you’ve got here.. It’s hard to find quality writing like yours nowadays. I truly appreciate individuals like you! Take care!!
Can I simply say what a relief to discover a person that really knows what they are talking about on the net. You certainly realize how to bring an issue to light and make it important. More people need to read this and understand this side of the story. It’s surprising you aren’t more popular given that you definitely possess the gift.
In the case that your body often tends in the direction of insulin resistance, that propensity will not ever vanish as well as the relevance of the difficulty with diabetic issues. A bariatric medical procedure could assist in lowering your blood sugar numbers and also you might reach a time where you do not need to take any kind of type of medications, yet you will constantly be required to understand that if you go back to the (prior) weight, the diabetes will possibly return. Article – http://aaslink.co/gastric
The beauty of direct VISCERAL or “belly” fat removal, is that if the patient eats excessively postoperatively (for psychological reasons rather than metabolic ones in view of the appetite stimulants (neuropeptide-Y and ghrelin) being reduced and resistin being reduced so that sugar can enter the brain and muscle cells), the fat will accumulate SUBCUTANEOUSLY on the hips, flanks and buttocks – WITHOUT dire metabolic consequences! The number of visceral fat cells are determined by genetics and diet during the first year of life. This fixed number of signet-shaped visceral fat cells fill up with fat, but don’t increase in number – EVER. Once removed, they don’t grow back. They are gone forever – permanently. The remaining fat cells may fatten up, but the mitochondrial apparatuses that secrete those bad cellular hormones is reduced and the risk of type 2 diabetes reduced forever. Intake of the sugar and salt of a bad diet may rev them back up into secretory mode again and raise the blood sugar, but never-the-less there will be fewer of them secreting, and a lowered tendency to type 2 diabetes.
In other words, visceral fat removal has a permanent effect compared to the other bariatric surgical alternatives which only STARVE the visceral fat and leave those evil visceral fat sells sitting there – flattened like sponges, waiting on the patient to break his/her diet with an intake of sugar and salt to fatten up again the return to the preoperative state. With EVL, those visceral fat cells removed at surgery are GONE FOREVER!
Before weight reduction surgical treatments, it is always desireable that non-morbidly obese individuals make a concerted effort to reduce a particular quantity of weight through eating routines, exercise and (often) medication.
Some such individuals may lose enough weight normally, that surgical procedure comes to be unneeded. — http://aaslink.co/gastric
However diet and exercise are generally unsuccessful in keeping weight off in the long term once homeostasis has been attained with substantial visceral fat present.